Ankle fractures are common injuries that can significantly impact an individual’s mobility and quality of life. There are various classification systems that we use to describe ankle fractures. The Weber classification is widely recognised and helps guide treatment decisions. In this blog, we will explore the different types of Weber ankle fractures and discuss their management strategies.
What is a Weber Ankle Fracture?
A Weber ankle fracture refers to a break in the fibula bone (the outer bone of the lower leg) near the ankle joint. The classification system is based on the level and direction of the fibular fracture in relation to the ankle joint.
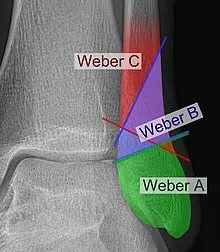
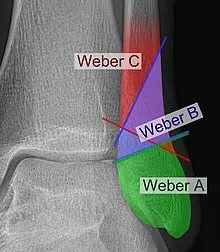
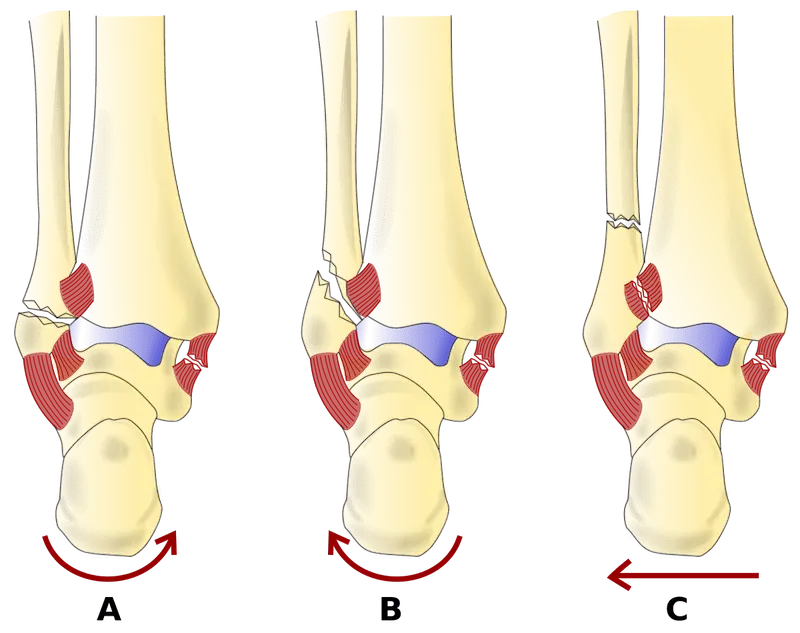
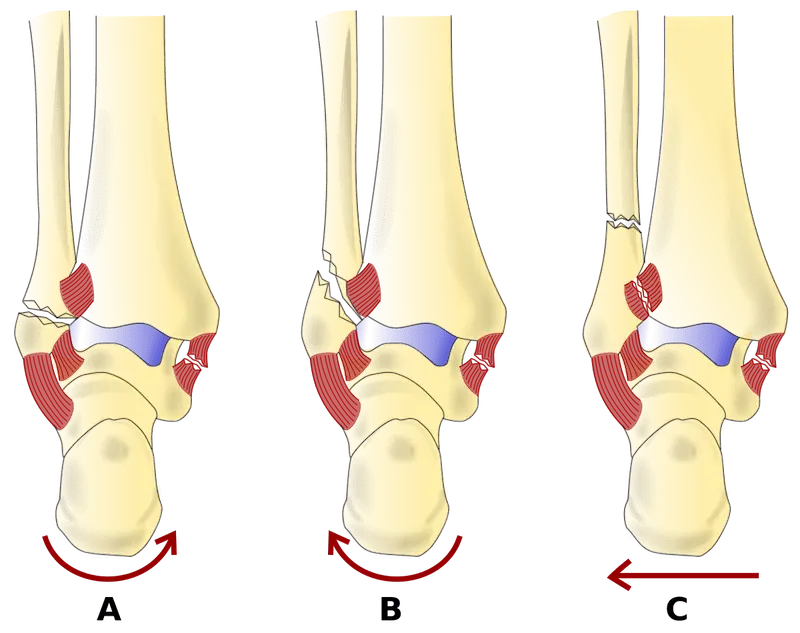
Type A Weber Ankle Fracture:
Type A fractures occur below the level of the ankle joint. These fractures involve the fibula and are typically stable, with minimal disruption to the ankle mortise (the joint formed by the tibia and talus). Treatment for type A fractures are usually conservative (physio and period of immobilisation).
Type B Weber Ankle Fracture:
Type B fractures occur at the level of the ankle joint itself. These fractures involve the fibula and may also involve the ligaments that stabilise the ankle joint. Type B fractures can be further subclassified as B1, B2, or B3, depending on the degree of ligamentous injury and joint instability.
- B1 fractures: These fractures are stable, with minimal or no ligamentous injury. Treatment typically involves non-surgical methods, such as casting or a moonboot, to immobilise the ankle and allow healing.
- B2 fractures: These fractures involve partial disruption of the ankle ligaments, resulting in mild to moderate instability. Management may include immobilisation followed by a period of protected weight-bearing or surgical intervention.
- B3 fractures: These fractures indicate complete disruption of the ankle ligaments, resulting in significant joint instability. Surgery is usually necessary to repair the ligaments and stabilise the ankle joint.
Type C Weber Ankle Fracture:
Type C fractures occur above the level of the ankle joint. These fractures involve the fibula, but they also include a fracture of the tibia (the larger bone of the lower leg) or disruption of the syndesmosis, the ligamentous complex that connects the tibia and fibula. Type C fractures often require surgical intervention to restore the anatomical alignment of the bones and stabilize the joint.
Management Considerations:
The management of Weber ankle fractures depends on various factors, including the type of fracture, associated injuries, patient characteristics, and functioning requirement. Treatment options may include conservative measures (period of immobilisation and physiotherapy) or surgical intervention (internal fixation, external fixation, or a combination of both).
Non-surgical management is generally suitable for stable fractures and fractures without significant joint involvement. Surgical intervention is typically considered for unstable fractures, cases with joint involvement, or when conservative measures fail to provide adequate stability.


Post-surgical rehabilitation is crucial to optimise functional outcomes. Physiotherapy is often required to regain strength, improve range of motion, and promote proper gait mechanics for full returning to work/activities.
Understanding the different types of Weber ankle fractures and their management approaches is essential for healthcare professionals and patients. The Weber classification system provides guidance in determining the severity of fractures and tailoring appropriate treatment strategies. Whether through conservative measures or surgical intervention, the primary goal is to restore ankle stability, promote healing, and facilitate a successful recovery, allowing individuals to regain their mobility and resume an active lifestyle.





