As physios, one of the most common conditions we see is plantar-fasciopathy. While many people still refer to it as plantar fasciitis, the medical community has evolved its understanding of this condition, leading to the more accurate term “plantar fasciopathy.” In this blog, we’ll delve into what plantar fasciopathy is, the causes, symptoms, and how to eradicate it.
What is Plantar Fasciopathy?
Plantar fasciopathy is a painful condition that leads to overload and thickening of the plantar-fascia. The plantar-fascia is a thick elastic band which connects form the heel bone (calcaneus) to your toes (pictured above).
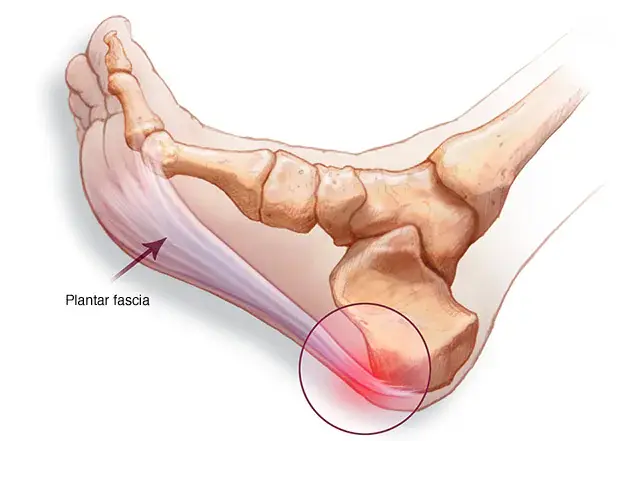
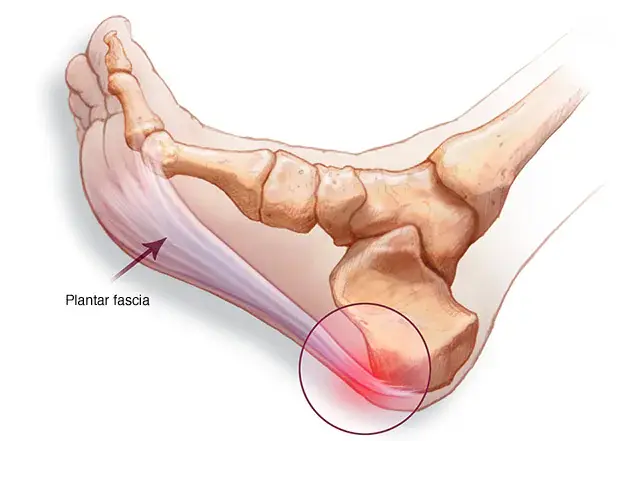
The plantar-fascia has 2 main functions:
- It acts as a shock absorber when walking and jumping. Essentially, any activity that requires landing on your foot.
- Its elastic properties act to propel you forward when walking, running, jumping. This then help you push further forward in a smooth way


Causes:
- Overuse: Plantar fasciopathy is frequently seen in individuals who have dramatically increase the load in a short period of time (playing multiple sports at once, increasing frequency of sports, etc.)
- Poor Foot Mechanics: Abnormal foot mechanics, such as flat feet or high arches, can increase the risk of developing plantar fasciopathy. Weakness in certain muscles, which then also places more load through the plantarfascia.
- Obesity: Excess body weight places additional strain on the plantar fascia, increasing the likelihood of developing this condition.
What you may be feeling:
The main symptoms that you may be feeling is heel pain, particularly when taking the first steps in the morning or after long periods of inactivity (sitting, standing). The pain may also intensify after physical activity. It often presents as a sharp, stabbing sensation in the heel or arch of the foot.
How can you get rid of this:
- Rest and Ice: Previously it was thought that rest was helpful. however, the most recent research shows otherwise. Instead of rest, research shows that strengthening the plantarfascia in a methodical and systematic way is what it needs.
- Stretching and Strengthening: In our team we are continuously searching and testing different muscles to determine which muscles are weak and may be placing extra load on the plantarfascia. Once we have determined the weak muscles, we can then prescribe specific exercises to strengthen them and reduce the load on the plantarfascia.
- Orthotics: Custom-made shoe inserts and heel gel pads can be helpful in providing additional arch support and correct abnormal foot mechanics.
- Footwear: Choose supportive, well-cushioned shoes with good arch support. Avoid wearing unsupportive footwear like flip-flops.
- Anti-Inflammatories, Cortisone Injections and Ice Therapy: previously it was thought that the plantar fascia was driven by inflammation. however, the most recent research shows that there is no inflammation present. So this is why anti-inflammatories, ice and cortisone injections are NOT helpful for this particular condition.
Plantar fasciopathy, formerly known as plantar fasciitis, is a common foot condition that can be painful and debilitating if not properly managed. Understanding its causes, symptoms, and treatment options is essential in order to provide good outcomes and helping you enjoy the things that you love with no pain.





